FAQ on COVID-19 Delta variant: symptoms, timeline, and transmissibility
The COVID pandemic is still going strong throughout all continents. Public health officials continue to exhort the same route to stay safe. Get vaccinated, wear a mask, and distance yourself from others while being in public. Despite the ongoing global relaxation of covid measures, new variants still come to light. The old ones are not yet gone as well. Up to date, the Delta variant takes credit for being the most dangerous.
What should you do about the COVID-Delta variant, and what do you need to know?
What is the Delta variant of COVID-19?
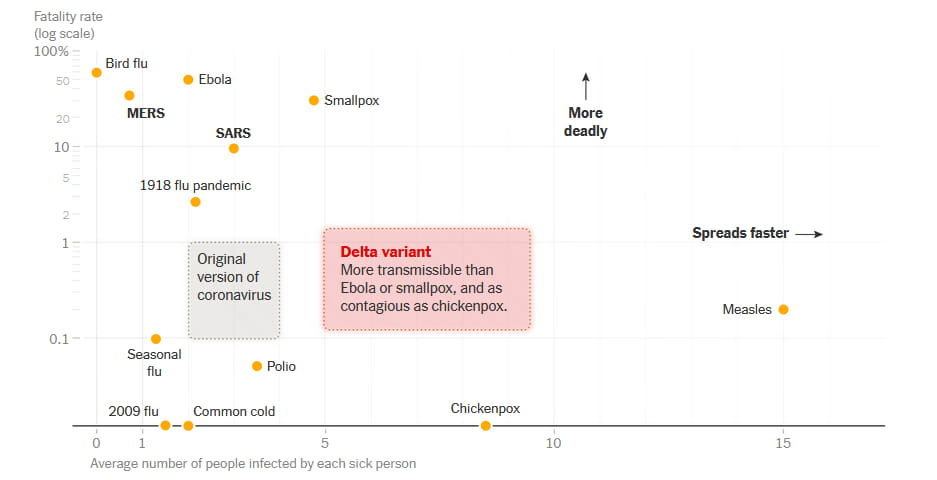
The delta variant was the third wave of COVID-19. It came in late 2020 as a new virus strain, more virulent than former strains. Essentially the same type of SARS-CoV-2 virus, but deadlier. The New York Times published a fatality rate report from the CDC to showcase how much deadlier.
As the virus hit the world with threatening rates of spread, officials did their best to counteract it. First boosters came by to fill the gaps for the new mutation in the current vaccines. Yet, experts found that the Delta mutation will break all established health barriers. All studies suggested a dominant projection of the Delta variant. Officials and people were looking for an explanation behind the Delta variant. All in an attempt to reduce the transmission of any coronavirus variants.
How is the Delta variant different?
The main problem with the coronavirus delta variant is speed. In the blink of an eye, hundreds of people can get infected from a single source. It isn’t due to increased longevity of the virus in the air, nor even due to a greater transmission distance. The delta covid type is identical to previous variants in all, but the spike protein.
You must have seen already the graphic model for the coronavirus molecule. The one that illustrates an orb with the protuberances growing out of it. Earlier COVID-19 incarnations share the same spiky outgrowths. But the Delta variant holds a slightly different shape, and the new shape is better at coming into contact with a potential host.
It latches on more tightly to the host receptor, so transmission from person to person becomes much easier.
Dr. Nasia Safdar, medical director of infection control at UW Health
It’s what makes it different and more contagious than its’ predecessors. But not invincible. Although not quite adapted to the subset at first, vaccines remain the only weapon to fight off COVID-19 up-to-date. Governments continue to invest in vaccination campaigns.
Even President Biden propagates further vaccination. He supported the effectiveness of vaccines against the delta variant – and newer – last summer:
Contagious effect of the Delta
The new delta variant is deadly, and the rise in the death rate is a good example. CDC and WHO experts suggest that the Delta variant originated in India in late 2020. Soon after it swept rapidly through the globe, accounting for more than 99% of COVID-19 cases at the time. The hospitalization rate was even higher than the Alpha strain.
In a completely unmitigated environment—where no one is vaccinated or wearing masks—it’s estimated that the average person infected with the original coronavirus strain will infect 2.5 other people. In the same environment, Delta would spread from one person to maybe 3.5 or 4 other people.
F. Perry Wilson, MD, Yale Medicine epidemiologist
That makes it about 100% more contagious than the original strain of SARS-CoV-2. In August 2021, the Journal of Travel Medicine published an average estimate for the Delta strain’ R0 of 5.08.
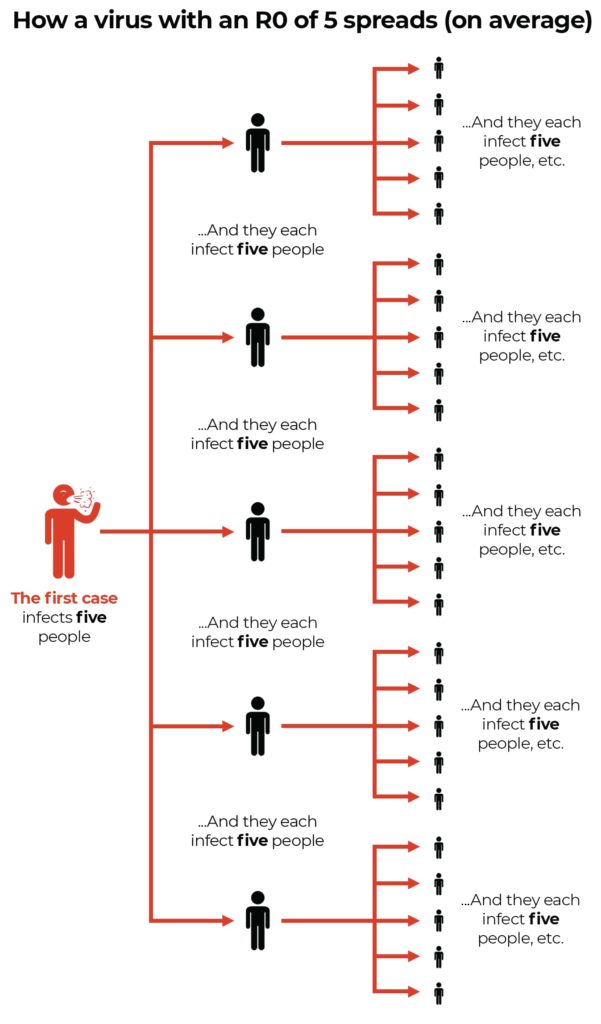
A reproductive number (R0) of 5.08 means each infected person transmits the disease to 5 people on average.
News coverage did a good thing emphasizing that by streaming the numbers. As a result, the world understood the Delta variant is contagious. For a reason. The Delta variant is more transmissible than the previous mutation.
What are the COVID-19 delta variant symptoms?
Usually, symptoms of Delta COVID are not disparate from symptoms of other variants. Unique about the type is the rare loss of taste and smell. Many people share common cold issues like sore throat, a runny nose, or a “funny off feeling”. That plays a bad joke as the younger population and people don’t realize how the virus goes undetected under the “bad cold” label. Nonetheless, associated with the Delta variant is a wider range of symptoms. Educating yourself about these might help you know when to get tested. As a rule, symptoms appear within one week after the infection. Yet, sometimes it may take up to a couple of months or longer to develop in some unlucky individuals.
According to the WHO, the prevalent symptom of the variant involves persistent coughing. So, a new extreme case of cough should raise your alertness. But coughing alone isn’t a set signal of coronavirus infection. Rarely ever it is the first one to come. The ZOE COVID project published results from their study of symptoms of coronavirus in more than 1M confirmed cases in the UK, as per which manifestations of the Delta type prove to vary between vaccinated and unvaccinated people.
Delta variant symptoms in adults
The top five signs for unvaccinated adults are:
- Headache
- Sore throat
- Runny nose
- Fever
- Persistent cough
Symptoms of delta in vaccinated people
The ranking changes after vaccination and looks like this:
- Runny nose
- Headache
- Sneezing
- Sore throat
- Persistent cough
The symptoms look similar for both fully vaccinated people and those who had only one dose. Still, distinction finds the top 2 indicators with swapped places for the latter.
First symptoms of delta variant
The number one symptom for the cases is a headache. It is then followed by a sore throat, a runny nose, and fever. Classic symptoms of the “traditional” coronavirus – such as cough or loss of smell – are much rarer with the Delta variant. That hides the infection and further makes the virus more contagious.
Dr. Mike Hensen’s brief explanation of this variant covers the above and other common symptoms.
Progression timeline of Delta COVID
The virus that causes COVID-19 is SARS-CoV-2. SARS-CoV-2 is spread by droplets released by infected people when they breathe, cough, or sneeze. Transmission can also occur when a person touches a contaminated object and subsequently touches their face. Regardless of the variant at large around the globe.
SARS-CoV-2 begins to reproduce once it enters your body, generally through your nose or mouth. The period from exposure to the virus being detectable by a PCR test is the latent period. For Delta, this is an average of four days.
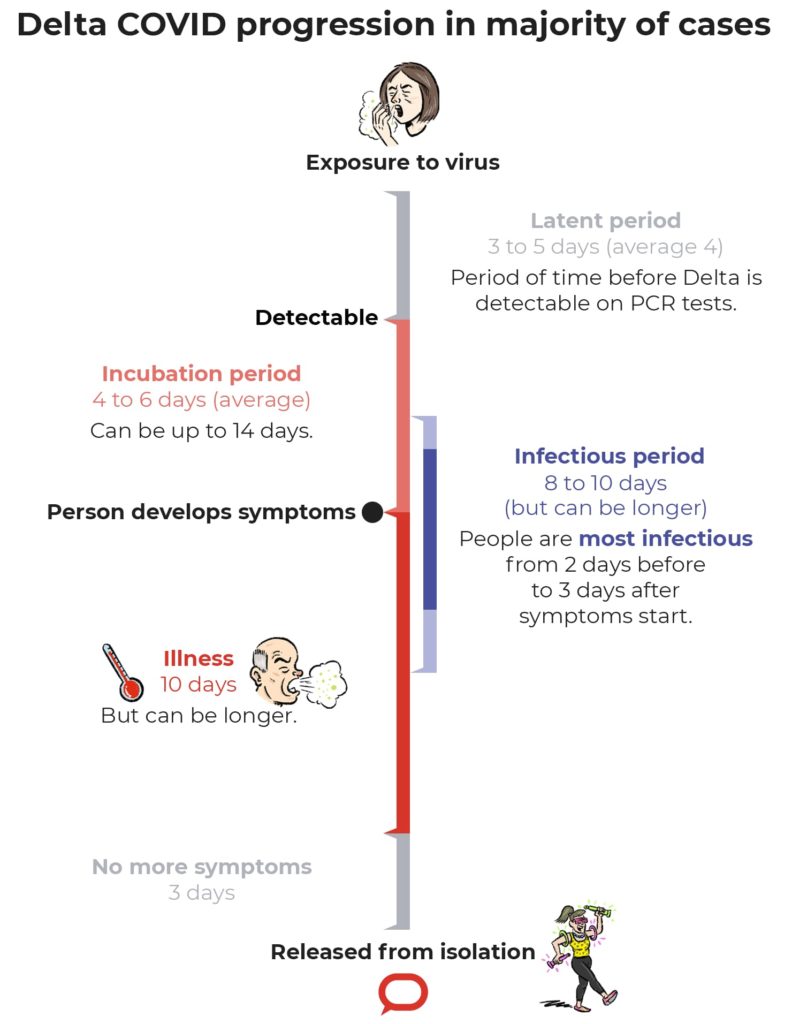
The incubation period is the time necessary for symptoms to develop and show, after exposure to the virus. With the Delta variant, this time reduces to 2-3 days, in comparison with 4-6 days with other types. The most contagious span is from 2 days before the beginning of the incubation period to 3 days after. The higher viral loads and faster replication rate of the virus lead to the rapid spread of the virus.
In plain English:
Someone who is sick with this virus produces a lot more of the virus, 100 to 1,000 times more virus in your nose compared to the prior strains and variants that we’ve dealt with. That hundreds or thousand times more virus means that each time you cough, sneeze, exhale, sing or yell at somebody, you’re putting more virus out there into the air. And that makes it more contagious.
Dr. John Vanchiere, director at LSU Health Shreveport’s Center for Emerging Viral Threats
Comparison with other variants of COVID-19
Studies suggest that the hospitalization rate for the Delta mutation equals 6.1% with a 1.6% chance of ICU admission. In comparison with former variants, which landed 5.4% of people in hospital, serves as a shred of evidence the subset makes people sicker. Another study revealed a 49% chance of developing pneumonia resultant of Delta. Out of those numbers, 28% required supplementary oxygen therapy as a treatment.
In a nutshell, emerging data indicate a higher possibility of severe disease with Delta. Approximately, doubled the risk of hospitalization, as opposed to the Alpha variant. And the Alpha proved to be 50% already more dangerous than the original strain.

Delta vs. Omicron
In November 2021, the WHO announced a new coronavirus variant of concern, named Omicron. This new variant was first reported in South Africa and soon unleashed a global outbreak. In a couple of months, the Omicron replaced Delta as the predominant variant. More than 30 countries reported confirmed cases of the new virus as of the beginning of 2022. Yet, the Delta variant is still under the variants of concern list of the WHO in April 2022. Despite the 2-3 times increased transmissibility rates of the Omicron, the Delta COVID is still riskier. A plethora of research teams dug into the severity of the newest coronavirus mutation. Early evidence forms 2 fundamental suggestions:
- Omicron is less likely to send patients to hospitals. Furthermore, if adults need hospitalization, they are less likely to be admitted to ICU.
- Omicron causes less damage to lung cells, resulting in less severe disease than the Delta.
Even so, the Omicron is still threatening senior members of the community. It is accounting for 20% more deaths in the age group above 75 than the Delta surge. Sometimes mild symptoms can develop into severe immune responses later.
It is still a coronavirus. We’re still in a pandemic.
Dr. Waleed Javaid, director of infection prevention and control at Mount Sinai Downtown in New York City
It is important to protect the risk groups of people. Such alarming data further emphasizes the importance of vaccination and boosters. It’s also crucial to stay home and get tested if you develop cold or flu-like symptoms.
Delta vs. Delta Plus
During the Delta surge, a new descendant, dubbed Delta Plus (AY.4.2), gathered global attention. This version, however, is not a devastating game changer. Rather a mild headache. For the most of it, there’s a huge amount of overlap between Delta and Delta Plus symptoms, virulence, and severity.
Can a vaccinated person spread Delta?
Findings show that vaccination alone is not enough to prevent transmitting of the SARS-CoV-2 Delta infection. An analysis of 621 people researched whether vaccination cuts transmission of the coronavirus Delta variant. Turns out, vaccinated people can hold as much viral load in their noses as unvaccinated ones. The analysis brings a collapse to all the theories for reaching herd immunity.
People who have a Delta virus and happen to have ‘breakthrough’ infections can carry these really high levels of virus, and can unwittingly spread the virus to others
David O’Connor, a virologist at the University of Winsconsin-Madison
What that means is the vaccinated people could be aiding the rise of the Delta surge. A gruesome statement that only underscores the importance of social distancing and masks. But while it can be true that vaccinated people can spread the virus, getting as many people double vaccinated could help reduce the overall number of confirmed cases in the first place. Controlling new coronavirus waves is challenging. But full vaccination and social distancing practices help keep the ones around you safer.
Reaching herd immunity with Delta – mission impossible
Sir Andrew Pollard, a chairperson of the JCVI, told lawmakers in the UK to stop working on the herd immunity approach. Reaching herd immunity through vaccination against COVID-19 is impossible. There will be new mutations that can spread faster than before and cause an even worse impact. But what renders the idea mythical is the fact that vaccinated people can get infected again. Those breakthrough infections mean that meeting the threshold for overall immunity won’t suffice. At some point, unvaccinated people might still contract the virus.
What is “herd immunity”?
Herd immunity is when the majority of the population is immune from a disease – via vaccines or by nature. In such a state, those who can’t get a vaccination or have a compromised immune system will be immune as well.
Scientists define steps for achieving herd immunity in three different ways:
- When a substance is entirely unavailable to infectious agents or non-infectious antigens. This means that the immune system can’t recognize them.
- There should be enough of an antigen present to prevent infection.
- Vaccination is at least 95% of people should prevent the disease.
Why herd immunity is unattainable?
SARS-CoV-2 proved that the population doesn’t have the ability to fight off an infection without developing symptoms. As each new mutation introduces newly infected cells to the body, it is impossible to reach the state of passive immunity. The only viable option could be through a massive vaccination campaign. But reaching herd immunity through vaccination against COVID-19 is difficult for many reasons.
- Vaccine skepticism for fear of possible complications or reluctance about the benefits is a good example.
- Breakthrough infections prove it is possible to get the virus again and spread it.
- Vaccine distribution disallows certain countries to have even access to COVID-19 vaccines. Even if a single community achieves local herd immunity, outbreaks from surrounding areas might disrupt.
